Diabetes Mellitus is a multifaceted metabolic disorder that has become a global health concern. With a rising number of cases each year, understanding its causes, diagnosis, and management is crucial.
This article delves deep into the intricacies of Diabetes Mellitus, aiming to provide a comprehensive overview for a diverse readership. Diabetes mellitus is a group of metabolic diseases characterized by high blood glucose levels.
This can be due to inadequate insulin production, improper response of the body’s cells to insulin, or a combination of both. The primary symptoms include frequent urination, increased thirst, and heightened hunger.
There are several types of diabetes, each with its unique causes and characteristics.
Types of Diabetes
There are primarily three main types of diabetes:
- Type 1 diabetes: This form arises when the body fails to produce insulin. It was formerly known as “Insulin-Dependent Diabetes Mellitus” or “Juvenile Diabetes”.
- Type 2 diabetes: This is the most common form and is characterized by insulin resistance. The body’s cells do not respond correctly to insulin, sometimes combined with an absolute insulin deficiency. It was previously termed non-insulin-dependent diabetes mellitus or “adult-onset diabetes”.
- Gestational diabetes: This type occurs in pregnant women without a previous diabetes diagnosis. It can lead to the development of type 2 diabetes later in life.
Other less common types include diabetes due to genetic defects of the beta cells, diseases damaging the pancreas, excessive amounts of certain hormones, and certain medications.
Symptoms
The primary symptoms of diabetes are:
- Polyuria: Frequent urination, especially at night.
- Polydipsia: Increased thirst.
- Polyphagia: Increased hunger.
- Weakness: A general feeling of being unwell.
- Weight loss: Unexpected weight loss and loss of muscle bulk.
- Other symptoms: Frequent episodes of thrush, slow-healing wounds, and blurred vision.
Type 1 diabetes can manifest rapidly, while type 2 diabetes symptoms might remain unnoticed for years.
Causes of Diabetes Mellitus

Understanding the causes of diabetes is crucial for its prevention and management.
Causes of Type 1
In type 1 diabetes, the body’s immune system attacks and destroys insulin-producing cells. This autoimmune response leads to an absence of insulin, causing an increase in blood glucose levels.
It is often termed insulin-dependent diabetes and usually develops before the age of 40.
Causes of Type 2
Type 2 diabetes arises when the body doesn’t produce sufficient insulin or when the body’s cells resist insulin, known as insulin resistance. Several risk factors contribute to the development of type 2 diabetes:
- Obesity or being overweight
- Impaired glucose tolerance
- High blood pressure
- Dyslipidemia
- Gestational diabetes
- Sedentary lifestyle
- Family history
- Age
Gestational Diabetes
During pregnancy, some women experience elevated blood glucose levels due to reduced insulin receptor sensitivity. This condition is termed gestational diabetes.
Diagnosis
Timely diagnosis of diabetes can prevent complications and improve the quality of life.
Blood Tests
Several blood tests can diagnose diabetes:
- Fasting plasma glucose: Measures blood glucose after an overnight fast.
- Two-hour postprandial test: Measures blood glucose two hours after eating.
- Oral glucose tolerance test: Assesses the body’s response to a glucose load.
Another crucial test is the Glycated Haemoglobin (HbA1c), which provides an average blood glucose level over the past 2-3 months.
Diagnostic Criteria
The diagnosis of diabetes is based on specific blood glucose and HbA1c levels:
| Condition | 2-hour plasma glucose | Fasting plasma glucose | HbA1c |
|---|---|---|---|
| Normal | <7.8 (<140) | <6.1 (<110) | <6.0 |
| Impaired Fasting Glucose | <7.8 (<140) | ≥ 6.1(≥110) & <7.0(<126) | 6.0–6.4 |
| Impaired Glucose Tolerance | ≥7.8 (≥140) | <7.0 (<126) | 6.0–6.4 |
| Diabetes mellitus | ≥11.1 (≥200) | ≥7.0 (≥126) | ≥6.5 |
Other Diagnostic Tests
Apart from the primary diagnostic tests, other tests can provide insights into the patient’s overall health:
- Fasting lipid profile
- Liver function tests
- Kidney function tests
- Thyroid-stimulating hormone (TSH) test
Management of Diabetes Mellitus
Effective management of diabetes is pivotal to ensure a high quality of life and prevent complications. It requires a combination of medical interventions and lifestyle changes.
Medications for Diabetes
Several classes of oral antidiabetic drugs (OADs) are available:
- Biguanides (e.g., metformin): These reduce the amount of glucose the liver releases into the bloodstream.
- Sulfonylureas (e.g., glimepiride): These stimulate the pancreas to produce more insulin.
- Meglitinides (e.g., repaglinide): These also stimulate the pancreas but are faster-acting and have a shorter duration.
- Thiazolidinediones (e.g., pioglitazone): These make the body’s cells more sensitive to insulin.
- Dipeptidyl peptidase IV inhibitors (e.g., sitagliptin): These help the body produce insulin in response to meals.
- α-Glucosidase inhibitors (e.g., acarbose): These slow down the body’s digestion of starchy foods.
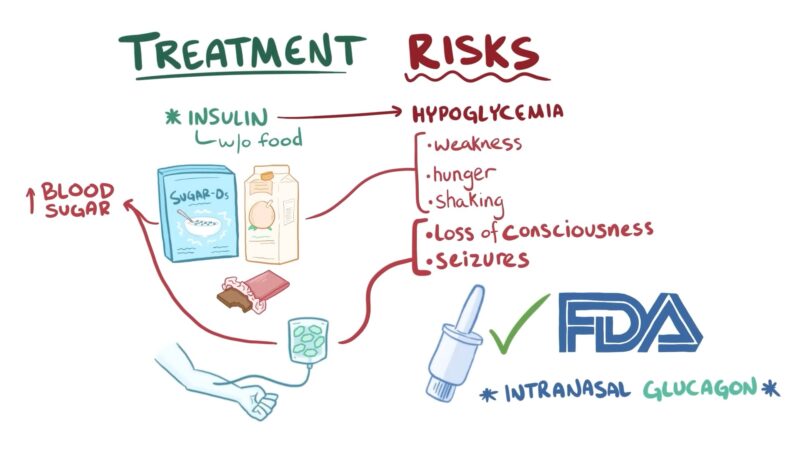
For those with Type 1 diabetes and some with Type 2, insulin injections are essential. Different types of insulin cater to various needs, from rapid-acting to long-lasting.
Lifestyle Measures
Lifestyle changes play a crucial role in managing diabetes:
- Regular exercise: Helps in maintaining a healthy weight and improves insulin sensitivity.
- Proper diet: A balanced diet with controlled carbohydrate intake can regulate blood sugar levels.
- No smoking: Smoking can exacerbate the complications of diabetes.
- Limiting alcohol: Excessive alcohol can lead to blood sugar spikes and drops.
Complications of Diabetes Mellitus
If not managed effectively, diabetes can lead to a range of complications, both acute and chronic.
Acute Complications
- Diabetic ketoacidosis (DKA): A severe condition where the body starts breaking down fat too quickly, leading to an accumulation of ketone bodies in the blood.
- Hyperglycemia: Extremely high blood sugar levels can lead to dehydration and an imbalance of electrolytes in the body.
- Hypoglycemia: Abnormally low blood sugar can result in symptoms like shakiness, sweating, and confusion.
- Diabetic Coma: A severe complication where high or low blood sugar levels lead to unconsciousness.
Chronic Complications
Chronic complications can affect various parts of the body:
- Microvascular diseases: These are due to damage to small blood vessels and can lead to:
- Eye Diseases: Such as retinopathy and macular edema.
- Neuropathy: Symptoms can range from tingling to numbness and pain.
- Nephropathy: Long-term kidney damage can lead to kidney failure.
- Macrovascular diseases: These affect larger blood vessels and can lead to coronary artery disease, peripheral arterial disease, and cerebrovascular disease.
- Other complications: It can cause or exacerbate certain skin infections, periodontal disease, and diabetic dyslipidemia.
FAQ
How does gestational diabetes affect future health?
Gestational diabetes can lead to the development of type 2 diabetes later in life.
What is the significance of the Glycated Haemoglobin (HbA1c) test?
The HbA1c test provides an average blood glucose level over the past 2-3 months, giving a broader view of blood sugar control.
Are there any lifestyle changes recommended for managing diabetes?
Yes, regular exercise, a balanced diet, no smoking, and limiting alcohol are essential lifestyle measures for managing diabetes.
What are the potential complications if diabetes is not managed effectively?
Unmanaged diabetes can lead to both acute complications like diabetic ketoacidosis and hypoglycemia, and chronic complications affecting various parts of the body, such as eye diseases, neuropathy, nephropathy, and cardiovascular diseases.
Final Words
Diabetes Mellitus, while a challenging condition, is not insurmountable. With the right knowledge, proactive management, and a commitment to a healthy lifestyle, individuals can navigate this journey with resilience and optimism.
It’s essential to stay informed, seek support, and prioritize one’s well-being. Remember, you’re not alone in this, and with the right tools and mindset, you can lead a life full of vitality and purpose.

